Advanced Treatment for Cervical Cancer Bangalore
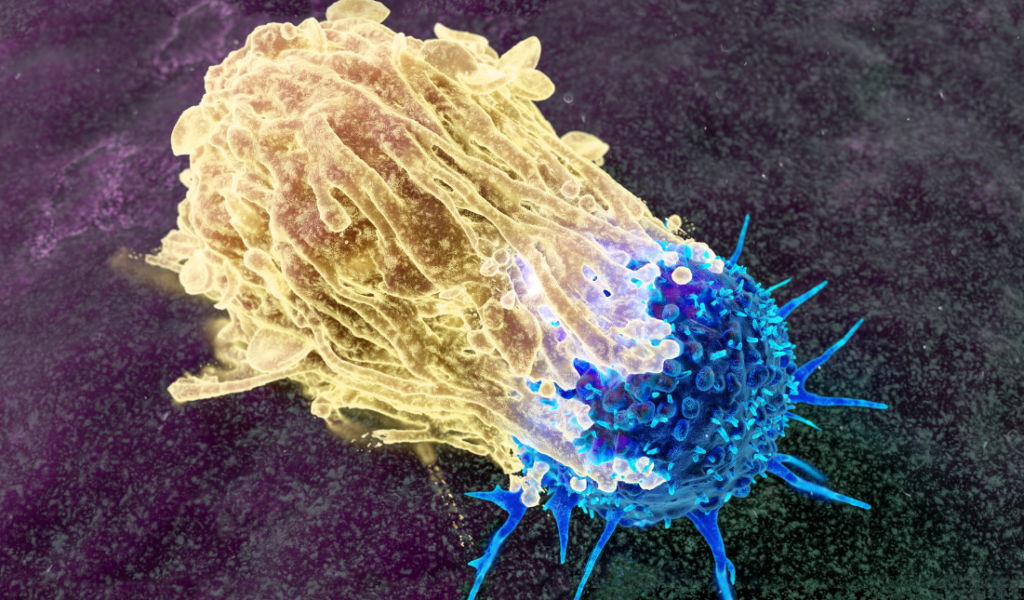
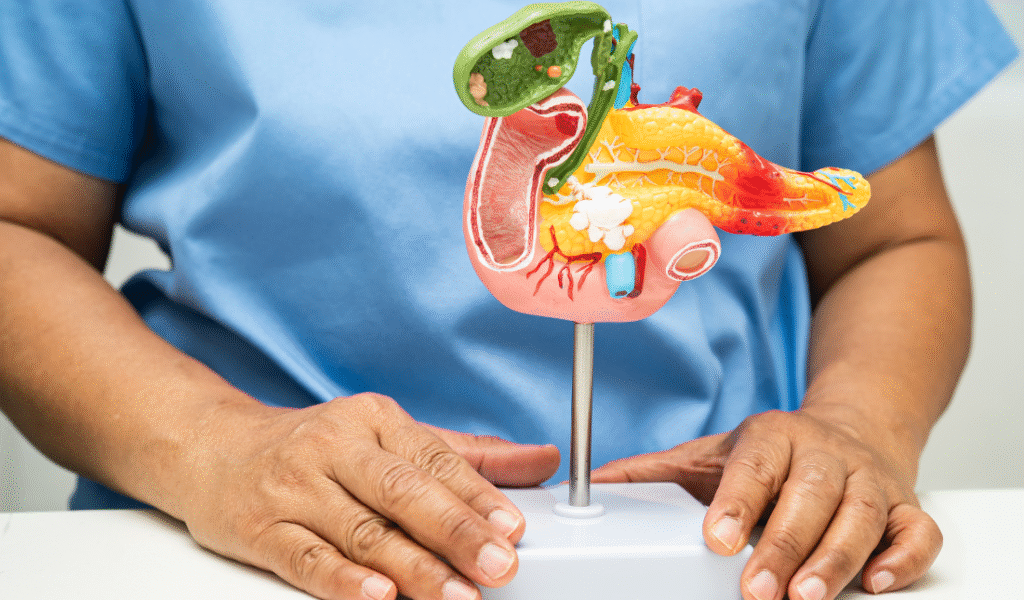
Advanced Treatment for Cervical Cancer Bangalore Book an Appointment Cervical Cancer: Preventable Today, Curable When Detected Early Cervical cancer begins in the cervix, the lower part of the uterus, and usually develops slowly over many years. Early abnormal cell changes often occur before cancer develops and can be detected through screening. Because early cervical cancer may not cause symptoms, prevention and early detection are the most powerful tools to reduce illness and death. At Healius Cancer Clinic, we are committed to changing the narrative around women’s health by providing the most advanced treatment for cervical cancer in Bangalore alongside world-class screening and treatment protocols. The Primary Cause: HPV The primary cause of cervical cancer is persistent infection with Human Papillomavirus (HPV). HPV is extremely common, and most infections clear naturally. However, certain high-risk HPV types can remain in the body and cause progressive damage to cervical cells, eventually leading to cancer if not detected early. The Burden in India India carries a significant share of the global cervical cancer burden, with approximately 1.2–1.3 lakh new cases and 75,000–80,000 deaths every year. Nearly 60–65% of affected women die, largely due to late diagnosis. These numbers underline the critical importance of vaccination, screening, and timely treatment at specialized centers like Healius Cancer Clinic. Prevention Through Vaccination – A Key Pillar Preventive (Prophylactic) HPV Vaccines HPV vaccines protect against the types most commonly responsible for cervical cancer. These are preventive, meaning they work best before exposure to HPV and do not treat existing infections. Healius Cancer Clinic provides access to leading vaccine brands: Gardasil® / Gardasil 9®: Protects against multiple high-risk HPV types and types causing genital warts. Cervarix®: Targets the two most important high-risk HPV types associated with cervical cancer. Recommendation: Vaccination is ideal between 9 and 14 years of age, before the onset of sexual activity, but can also be given later based on medical advice. Screening and Early Detection Even vaccinated individuals need screening. Regular Pap smears and HPV testing can detect abnormal cells before they become cancerous. Regular screening at our Bangalore clinic significantly lowers cervical cancer incidence and mortality. Advanced Cervical Cancer Treatment in Bangalore At Healius Cancer Clinic, treatment is planned by a multidisciplinary oncology team based on the stage, tumor size, and the patient’s fertility wishes. Surgical Treatment Surgery is the main treatment for early-stage disease. Options include: Conization or Simple Hysterectomy: For very early cases. Radical Hysterectomy: Removal of surrounding tissues and lymph nodes for slightly more advanced early stages. Radical Trachelectomy: A fertility-sparing surgery for young women who wish to preserve their ability to conceive. Radiation Therapy Radiation plays a major role, especially in locally advanced disease. We utilize: External Beam Radiation Therapy (EBRT) Brachytherapy: Internal radiation placed close to the cervix. Modern techniques at Healius allow for precise targeting, protecting organs like the bladder and bowel. Chemotherapy and Targeted Therapy Concurrent Chemoradiation: Giving chemotherapy with radiation is the standard for locally advanced stages. Targeted Therapy: Uses drugs that inhibit tumor blood vessel formation (angiogenesis), starving the tumor of its blood supply. Immunotherapy: Helping the body’s immune system recognize and destroy cancer cells, especially in advanced or recurrent cases. Genetic and Molecular Insights Cervical cancer is primarily driven by HPV-related genetic damage rather than inherited mutations. Unlike breast or ovarian cancer, it is rarely hereditary. HPV infection remains the dominant risk factor, making it a disease that is largely preventable through lifestyle and medical intervention. Building Awareness for a Healthier Future Awareness among school children and the general public is essential. By understanding that cervical cancer is preventable, we remove the fear and stigma around women’s health. As emphasized by the World Health Organization, cervical cancer can be eliminated through widespread vaccination and screening. Healius Cancer Clinic stands as a partner for women in Bangalore, protecting future generations through education and early medical care. Take Charge of Your Health Today Don’t wait for symptoms to appear. Whether you need an HPV vaccination for your child or a screening for yourself, our experts are here to help. Healius Cancer Clinic – Bangalore Contact Us: +91 9900613143 Website Link: https://healiuscancerhematology.com/
Advanced Treatment for Cervical Cancer Bangalore Read More »